Sensory alalia, or receptive, impressive - underdevelopment of speech due to impaired auditory perception with normal physical hearing. A child with this pathology does not understand spoken speech, does not distinguish between sounds, and does not have phonemic hearing. He also has other disorders.
It is rare in its pure form, but nevertheless requires the intervention of a speech therapist, defectologist and neurologist and timely correction. In the article you will learn the causes of the disease, treatment and prognosis of sensory alalia.
Causes of sensory alalia in children
Sensory alalia is associated with damage to those areas of the brain that respond to the analysis of sounds and speech. To be more precise, the posterior third of the left hemisphere: it is projected onto the area behind the ear.
The disease is caused by:
- Pathology during pregnancy - intrauterine hypoxia, infections, immune attack, drug use, bad habits, harmful working conditions, intoxication;
- Damage to the central nervous system during childbirth: rapid labor, narrow pelvis, obstetric care. The consequence is traumatic brain injury. And protracted labor, entanglement of the umbilical cord, oligohydramnios, premature loss of water causes damage to brain cells due to insufficient oxygen supply - hypoxia;
- Pathology in the postpartum period and the first years of life - injuries, space-occupying formations, inflammatory and infectious diseases of the brain and meninges, intoxication, toxic damage to brain cells due to infectious diseases.
Most often, several factors influence a child. The cortical part of the auditory-speech analyzer is affected, and the process of recognizing sound stimuli is disrupted. The child hears speech, but cannot grasp its meaning and content. That is, he has not developed phonemic processes and does not have the skill of holistic speech perception.
As a result, the excitation (impulse) is not transmitted along the chain to other analyzers: speech-visual, speech-motor. Thus, the baby hears speech, but cannot perceive it, analyze it, and therefore does not react to it in any way.
Motor alalia.
Motor alalia (a. motoria; lat. motor motor) is an underdevelopment of expressive speech, expressed in the difficulty of mastering an active vocabulary and grammatical structure of the language with a fairly intact understanding of speech. Motor alalia is based on a disorder or underdevelopment of the analytical-synthetic activity of the speech motor analyzer, expressed, in particular, by the replacement of subtle and complex articulatory differentiations with coarser and simpler ones.
Causes of motor alalia.
The cause of motor alalia is damage to the cortical end of the speech motor analyzer (Broca's center) and its pathways, or a decrease in the functional activity of this center.
Motor alalia develops when the functions of the fronto-parietal areas of the cortex of the left hemisphere of the brain (Broca's center) are impaired and manifests itself in a violation of expressive speech with a fairly good understanding of addressed speech, late formation of phrasal speech (after 4 years) and poverty of pre-speech stages (frequent absence of babbling) . Accompanied by a gross violation of the grammatical structure (lack of agreement of words in gender, case and number, incorrect use of prepositions, absence of verbal forms in speech, rearrangement of syllables and sounds within a word, etc.). There is a pronounced poverty of vocabulary.
Motor alalia underlies disorders of school skills such as dyslexia and dysgraphia, as well as disorders of spatial gnosis and motor disorders such as apraxia; it is combined with local and diffuse neurological symptoms and damage to the structures of the dominant hemisphere, which determines the possibilities of expressive speech. In the mental state of children with a similar disorder, there are often manifestations of varying degrees of severity of psychoorganic syndrome in the form of motor disinhibition, attention and performance disorders in combination with intellectual development disorders.
Signs of sensory alalia in children
The main symptom of sensory alalia is misunderstanding of addressed speech of varying degrees:
- Easy degree - children understand simple words that are often used in everyday life and in familiar situations. At the same time, if the same word is heard in an unfamiliar environment, they cease to understand it;
- The average degree is accompanied by more severe disorders. The number of words to which the child somehow reacts is minimal;
- In severe cases, children absolutely do not respond to speech and even to their name.
In this case, a characteristic symptom of sensory alalia is verbosity (logorrhea) - active speech, rich in sound combinations and interjections. Usually it is incomprehensible to others. Also, one of the signs of the disease is uncontrolled repetition of words (echolalia). But if you ask the baby to say this word, he will not be able to do this purposefully.
The child’s process of correlation between a phenomenon or object and the word that denotes it is disrupted. He places accents incorrectly, replaces letters, or skips them.
The voice is clear, hearing and intelligence are preserved. The baby quickly loses interest in activities and games, and has an unstable mood. In general, he is uncontrollable, impulsive, and even sometimes aggressive. As a result, it is difficult for him to build communication with others, and those around him avoid him.
Types of pathology
Effective treatment of alalia in children is possible only after its type has been established. There are three main types in total.
Sensory alalia is a complex problem, so treatment for sensory alalia is always long-term. The term refers to speech disinhibition in the absence of perception of the speech of other people. This type of disease manifests itself in the fact that the child can speak for a long time, quickly, not always clearly and does not respond to speech addressed to him due to damage to the speech-hearing analyzer. Information reaches the child's brain in fragments; sometimes he is not able to understand even his own name, sometimes he understands individual words, but does not perceive the meaning of the phrase. In certain situations, children with a sensory type of illness can understand and follow simple instructions (for example, take soap and wash their hands), but in others even this does not happen.
Motor alalia is a specific condition, therefore the treatment of motor alalia in children requires an integrated and systematic approach. With this type of illness, the baby perceives the speech of other people addressed to him, but his speech skills are completely or almost completely absent. The child knows quite a lot of words, he correctly shows the objects that are named to him, but he himself finds it difficult to pronounce even simple and well-known words. It is difficult, and sometimes even impossible, for a child to simply repeat words after an adult - when pronouncing a word, he “loses” sounds and rearranges syllables. It is especially difficult for such a child to learn generalization words (chicken, crow, bullfinch - birds; soup, porridge, bread - food; mother, father - parents) and words - abstract concepts (anxiety, beauty, kindness). Correction of alalia, treatment and prognosis of motor alalia largely depend on how timely the parents turned to specialists.
Mixed (sensorimotor) type of disease . With the development of this type of pathology, the child does not speak (or almost does not speak) and does not perceive the speech of others. If alalia is not treated on time, then in almost 100% of cases, a child with a mixed form of the disease also develops delayed intellectual development.
Complications of sensory alalia
Impaired sound perception leads to incorrect pronunciation and unformed expressive speech. An additional symptom of sensory alalia is general speech underdevelopment. It is difficult for such children to master school material due to disorders of learning skills - impaired writing and reading. They find it difficult to communicate with peers.
In later life, this causes signs of psychological disorders and emotional and volitional disorders. The intellect suffers and mental retardation develops. Children become unsociable, withdrawn, and live in their own little world.
Alalia forms
Alalia is a severe impairment of speech functions or complete absence of speech. The reason for this lies in the delay in the maturation of nerve cells in certain areas of the cerebral cortex. The feature can be either congenital or acquired in the first three years of life - the conditional pre-speech period, when the active formation of cells in the cerebral cortex occurs. The main difficulty is that this is not a functional time delay, but a systemic problem that affects all components of speech. Elimination will require intensive, long-term work with a qualified specialist. There are three main forms of alalia.
Diagnosis of sensory alalia in children
Due to the diversity of the causes and mechanisms of development of the pathology, the diagnosis of sensory alalia consists of two parts: a medical examination and a psychological and pedagogical consultation. The medical part is aimed at identifying organic brain damage, neurological, mental disorders, diseases of the ear, nose and throat, which are characterized by lack of speech.
The examination is phased and includes:
- Neurological research methods - examination by a neurologist, analysis of the course of pregnancy in the mother, childbirth and the early postpartum period. The doctor examines the child’s outpatient record, specialist reports in the first year of life, and identifies previous diseases. Looks at the results of analyzes and instrumental research methods. If necessary, the neurologist prescribes skull radiography, echoencephalography, electroencephalography, MRI or CT scan of the brain;
- Examination by an ENT doctor to exclude organic damage to the organ of hearing and congenital deafness. Audiological diagnostics, audiometry, and tympanometry are performed. The child is cared for by an otorhinolaryngologist, and sometimes an audiologist is involved;
- Consultation with a speech therapist is one of the important parts of diagnosing sensory alalia. The specialist comprehensively studies the characteristics of speech, identifies early speech and neuropsychic development. Evaluates impressive speech, that is, speech understanding. The specialist gives simple commands that the baby must follow: show an object, make some movement, repeat syllables or words. These methods allow the speech therapist to understand the nature of the disorders;
- A consultation with a psychologist is necessary to assess the state of auditory-verbal memory, the baby’s behavior, and identify deficits in mental functions. Based on the obtained picture, the specialist determines the tactics for managing the patient.
In most cases, several consultations with specialists are required. This is due to the variability of the clinical picture with sensory alalia: sometimes the child easily gives in to contact, sometimes he refuses to communicate.
Also, the difficulty of diagnosis is associated with the need to exclude other speech disorders and mental disorders. For example, it is necessary to exclude autistic disorders, sensorineural hearing loss, aphasia, and mental pathology.
Diagnosis and treatment
You should consult a doctor if, when your child reaches 3 years of age, you notice that his speech is not developed enough. Even active treatment, but at a later age, may not give the expected results.
Alalia is a dangerous disease that can lead to mental retardation. In some cases, pathological personality traits and character formation of a neurotic type may develop. Children with motor alalia show isolation, lack of self-confidence, irritability, touchiness and a tendency to cry.
To overcome the disease as quickly as possible, you should listen to the recommendations of specialists: everything that the doctor prescribed must be done in full and on time.
Diagnosis of the disease should be carried out by specialists. It includes electroencephalography, echoencephalography, skull radiography, MRI.
To determine the form of the disease, otoscopy and audiometry are also performed.
The speech therapist evaluates auditory-verbal memory and speech. A neurologist, otolaryngologist and psychologist are also involved in the work.
Treatment of sensory alalia in children
Treatment should be started as early as possible, before speech disorders are established and there are no severe psychological disorders. The role of family and loved ones is important: parents must understand the seriousness of the disease and be aware of the plan and stages of treatment. They are informed about the results of treatment at each stage. If necessary, a psychologist additionally works with them: for motivation, creating a favorable psychological background in the family.
Treatment is the same step-by-step process as diagnosis and consists of several parts:
- Medical methods of therapy include the prescription of drugs with nootropic effects, neuroprotectors, and vitamins that affect the central nervous system. Physiotherapeutic techniques (microcurrents, electrical stimulation, magnetic therapy), massage, therapeutic baths, and therapeutic exercises allow you to consolidate the effect of medications. How to treat sensory alalia depends on the individual characteristics of the baby and the course of his illness: there is no universal method or scheme;
- Classes with a speech therapist allow you to develop auditory perception and the ability to analyze speech. The specialist first works with logorrhea - verbosity, helps the child concentrate and maintain attention, teaches the skills of joint games and other team activities. The baby learns to distinguish non-speech sounds, then correlate sounds and short words with objects and actions. It is important that during the lessons the teacher clearly, understandably and briefly formulate the tasks and explain the material in the same way. Literacy training is of greater importance: the development of the visual analyzer facilitates the understanding of speech;
- Psychological assistance consists of developing thinking, memory, attention, and cognitive abilities. The specialist teaches the child skills to control emotions and corrects behavior. In a word, it helps him socialize.
Therapy for sensory alalia is usually long-term, continuous, lasting up to 4 years. After recovery, the child is observed. It is recommended that kindergarten and school continue classes with a speech therapist to prevent relapses and consolidate the results of treatment.
Corrective classes for child speech development
The basis for correcting speech disorders with signs of sensorimotor alalia in children is working with a speech therapist or speech pathologist. Group classes are possible, but at the initial stage it is better to study individually.
The specialist helps step by step:
- at the first stage, teaches how to correctly perceive and reproduce sounds and words;
- The second stage of therapy is aimed at constructing words and short phrases and developing dialogue skills. At the same time, the set of words in the lexicon is enriched;
- The third stage of correctional work consists of developing monologue speech and consolidating grammar.
Classes are conducted in a playful way, using toys and pictures. Usually the baby undergoes therapy on an outpatient basis. But in more complex cases, hospitalization in specialized hospitals is indicated.
It is useful to develop fine motor skills. Drawing, classes with construction sets, mosaics, modeling, and appliques are suitable for these purposes. Alternative methods include hydrotherapy (hydromassage, swimming pool, therapeutic baths), and treatment with animals (dolphin therapy, hippotherapy).
A psychologist also works with the child. Under his control, the baby learns communication skills and control of the emotional and volitional sphere.
Prognosis and prevention
The prognosis for sensory alalia depends on the timeliness of starting therapy. With a mild degree of impairment, active participation of parents in correction, and regular classes with a speech therapist, the result will be good. Speech disorders are eliminated and complications are prevented. The child acquires communication skills, communicates freely with peers, and can master the school curriculum.
With late treatment and lack of proper attitude on the part of parents, lack of regularity of classes, recovery is in question, unfortunately.
Prevention of sensory alalia
Prevention of speech disorders, as well as other health problems, begins at the stage of pregnancy planning. A woman needs to undergo diagnostics to identify health problems. Then correct the detected violations. Only after this can you plan to conceive.
During pregnancy, it is important to follow the doctor’s recommendations: undergo examinations and tests on time. If necessary, take medications and vitamins. Lifestyle and nutrition play an important role - a pregnant woman and her unborn baby need food rich in vitamins and microelements, adequate sleep and rest, and fresh air for proper development. Stress, intoxication, bad habits, and work in hazardous working conditions should be excluded.
It is necessary to prevent damage to the central nervous system during childbirth, in the early postnatal period and the first year of life.
Parents need to be especially careful if there is a person in the family with speech impairments. Children, especially small ones, repeat with adults: in this way he can copy an adult who speaks poorly or does not speak at all.
We also want to draw parents’ attention to the fact that sensory alalia does not go away on its own in children. This is a serious speech therapy, psychological, and sometimes psychiatric pathology with many causes, which can only be overcome with the joint efforts of doctors, parents and the child himself. Therefore, we recommend that you contact a specialist as soon as possible if signs of sensory alalia are detected and begin treatment.
Alalia are linguistic disorders of speech activity, i.e., symbolic, amodal, and not a direct consequence of pathology of the sensory or motor spheres.
Impressive (sensory) alalia syndrome is otherwise called a specific disorder of receptive speech development (F80.2 according to ICD-10). With this syndrome, a child without visible intellectual impairments, who has sufficient hearing, does not begin to understand spoken speech in time and, as a result, speak.
Diagnosing impressive alalia can be difficult. A number of authors [1, 2] indicate that sufficiently clear, unambiguous diagnostic criteria have not been developed for impressive alalia. Moreover, its very existence as an independent disorder is not recognized by everyone.
Children with alalia from the very beginning acquire language according to a pathological type, which distinguishes them from children with delayed language acquisition, in which language is formed later than usual, but according to the laws of the norm [3]. There are two main forms of the disease: expressive (EA) (motor) and impressive (IA) (sensory). Sometimes they talk about sensorimotor alalia, emphasizing that the clinical picture includes disturbances in both understanding and speaking. In our opinion, in almost every case, both impressive and expressive speech suffers. T.G. Wiesel [4] wrote that since expressive and impressive speech in a child are closely related, as a rule, with both forms of alalia, there is a deficiency of both types of speech activity. Moreover, with any of the forms, with motor alalia, secondary difficulties in understanding can be mild, and with sensory alalia, secondary disturbances in one’s own speech can be severe, even to the point of its absence.
Impairments in speech understanding in IA and EA, in our opinion, differ not quantitatively, but qualitatively. Thus, children with EA often have difficulty understanding grammatical structures. It is also difficult for them to distinguish by ear words that sound similar. At the same time, with severe EA and intellectual development disorders, understanding the general meaning of statements remains accessible [5, 6]. For I.A. characterized by a lack of understanding of the general meaning of statements, including the simplest everyday speech, as well as uncriticality of one’s speech. Similar disorders occur in the clinic of aphasia due to brain damage, but only in the acute period. Persistent impairment of speech understanding, similar to IA, is observed in Landau-Kleffner syndrome (LKS), according to ICD-10 F80.3.
The idea of alalia as a childhood analogue of aphasia, caused by brain damage in Broca's or Wernicke's areas, is not confirmed today in children with alalia: in the vast majority of cases, focal brain lesions are not detected. Conversely, children who had brain lesions at an early age develop not alalia [7-11], but childhood aphasia, i.e., disorders of formed speech that tend to quickly restore verbal communication [12, 13]. Recent studies of the formation of more complex language skills in this category of children at school age have revealed [14-17] the presence of certain impairments compared to controls, but in the light of our work, it is important what these children say. Based on these facts, it is logical to assume that alalia is not a manifestation of any residual damage to the child’s brain. In children with cerebral palsy, alalia is observed only in 3.8% of cases, although this may be due to diagnostic difficulties [18].
Various aspects of EA are presented in the works of a number of authors [1–3, 19]. The nature of brain damage in IA will be discussed further. Based on the clinical observations of N.N. Traugott and S.I. Kaydanova [20] came to the conclusion that in children with sensory alalia and aphasia (children’s sensory aphasia, which the authors call SLC), the higher speech areas of the brain remain open, as in adults with sensory aphasia, the formation and consolidation of conditioned connections to sound is selectively impaired irritants with the formation of “functional inferiority of the higher levels of the auditory system or central hearing defect.” The authors proved that the defect in auditory function in IA cannot be reduced to a violation of physiological hearing.
The diagnosis of IA can be made based on observation, with the main symptom being the absence of speech understanding at the age of 18 months without significant reduction in physiological hearing and visible impairment of intelligence. Speaking about IA, one cannot help but draw a parallel with the well-studied SLE, which is interpreted as dysfunction of the temporal regions of the brain due to epileptiform activity [21–25]. In SLS, a previously normally developing child loses the ability to understand spoken speech and, consequently, to speak. Hearing and non-verbal intelligence are not affected. Loss of language ability can occur gradually, but more often it occurs suddenly. The average age of onset of the disease is 3-7 years. Numerous studies of CLS confirm the connection, in many cases direct, between cognitive impairment and epileptiform activity [26–30]. At the onset of SLS, there is not always a clear connection between changes in the EEG and speech regression: one event may precede another by a period of several months to 2 years. In adolescence, the EEG normalizes, but this is not always accompanied by the restoration of cognitive functions. In 2/3 of sick children, a pronounced defect in speech function remains, 1/3 completely recover.
The clinical manifestations of LSK with onset in preschool age and IA are almost identical and differ only in a vague age limit (before the appearance of speech - alalia, loss of formed speech - LSK). Moreover, these are the only known syndromes in which the leading symptom is a persistent misunderstanding of spoken speech. The work mentioned above [20] showed the identity of the disturbance in the formation and consolidation of conditioned connections to sound stimuli in IA and SLS. Diagnosis of SLS is based on EEG examination data. Moreover, SLS can act not only as aphasia, but also as alalia [26, 31—34], i.e., there is no doubt that some cases of IA are associated with pathological changes in the electrical activity of the brain. At the same time, not all cases of IA show abnormalities on the EEG. This gives reason to assume the possibility of brain dysfunctions of different nature, which manifest themselves in a similar clinical picture, i.e., with different etiologies, symptoms of prolapse are common due to the involvement of the same regions of the brain.
The question of what primarily suffers in IA, auditory gnosis or auditory agnosia, inevitably leads to severe underdevelopment of the language system, since at an early age the formation of gnostic and linguistic functions is closely related.
Impressive vocabulary in healthy children develops from 9-10 months [35]. At this time, the child begins to relate what he hears to relevant objects and situations. An active vocabulary begins to form between 10 and 18 months. In the case of IA, the child does not begin to understand the speech of others, an impressive vocabulary is not formed, and therefore conversational speech does not develop. At what point speech understanding is impaired in IA is unclear. At an early age, children behave appropriately to the situation, their behavior is guided by facial expressions, gestures, intonations of adults or they copy the behavior of their peers, and parents most often claim that their child “understands everything, but does not speak.” N.N. Traugott [6], describing the behavioral characteristics of children with IA, believes that their general pattern of behavior does not differ from their normal peers, they are proactive, and quite sociable.
We analyzed the symptoms and course of the syndrome in 17 children aged 2 to 10 years, some of them we describe below.
Observation 1
Boy, 3 years 5 months, sees a speech therapist for the first time. Entering the office, I rushed to the manuals that do not require verbal understanding (boards with slots for different figures), and began to collect them. He did not respond to questions and requests. However, when the teacher managed to turn the child to face him and point to the lamps on the ceiling and the switch, he realized that he was being asked to turn on the light and rushed to carry out the assignment. When they gestured to the table where there was a bear, a ball and a hare, and asked for the bear, he headed towards the table and stopped indecisively. He looked back at the adults, as if asking what exactly should be brought, and, not understanding the instructions, took all three toys.
The above example shows that children with uncomplicated IA at the age of 2-3 years do not understand the simplest verbal instructions and do not know the names of objects, but they understand gesture instructions and readily carry them out, communicate with gestures and generally behave like healthy children who are in unfamiliar language environment.
The general and speech behavior of children with an uncomplicated form of IA aged 4 years and older is characterized by high speech activity, contact, echolalia and the ability to name when they are unable to recognize the same word by ear.
Observation 2
Girl, 4 years 1 month, from a Russian-speaking family living in Germany. Entering the office for the first time, she extended her hand, smiled and uttered a long, inarticulate “phrase.” Interrupting the mother, she began to explain something, but the child’s speech was a “speech salad” in which syllables and whole words could be heard. She often answered “yes” to questions without understanding them. Of the six subject pictures, I was able to show only one by name. She pointed to the picture several times and clearly pronounced “dog” syllable by syllable, but after a few minutes she could not show this picture by name. When called by name, she turned around (perhaps this was a reaction to the vocative intonation). The parts of the face on the doll are readily shown, but only in the sequence “eyes, nose, mouth.” When the sequence changed, she could not show it, i.e. she did not understand these words. Instead of “legs” she showed “nose” twice, instead of “jacket” - “duck”, i.e. the child has already begun to focus on auditory perception, but the auditory image of the word is still inaccurate and approximate. Repetition: vowel sounds, syllables and simple words were sometimes repeated correctly, but more often with distortions. I enjoyed drawing. While drawing, she did not answer questions, but repeated them like an echo.
It is typical for children with IA not to pay attention to verbal messages and not to look at their name. At the same time, they react to slight noise outside the window, quiet steps along the corridor, etc. This distinguishes them from children with hearing loss.
After 3 years, children with IA often begin to point to pictures themselves and listen to the answer. This behavior probably reflects both the child's developing cognitive activity and a response to the actions of adults who have repeatedly attracted the baby's attention by pointing to an object and naming it. If parents are attentive and support the child’s activity, then soon we can expect that the meaning-sound connection for the first words will be established. Some children with alalia initially understand words and can only identify them by name if they are spoken by a familiar voice.
Children with IA often say something, accompany the games with “speech”; in the flow of their “speech” you can sometimes hear fragments of words and whole words, in some cases - only fuzzy sounds. This “speech” has no meaning, but melodically resembles phrasal speech. N.N. Traugott [6] draws attention to the similarity of the “speech” of children with alalia with the speech production of adult patients with sensory aphasia, which is called “word salad.”
This symptom in patients with sensory aphasia can be observed only in the acute period of the disease; later, criticism of one’s speech is restored. The first meaningful words are usually the names of objects. Feature I.A. - active vocabulary exceeds passive - is associated with inferiority and instability of auditory perception: the child can name an object, therefore the sound-meaning connection is established, but when perceiving a familiar word by ear, it is not always recognized. The most important role in the process of understanding speech in such patients is played by voluntary attention: if the child is “switched on,” he performs tasks.
The phenomenon of echolalia is well known in IA. It usually manifests itself as a repetition of a question addressed to the child. Sometimes the child repeats only those questions that are addressed to him, as if trying to answer, and in some cases he spontaneously repeats everything he hears around him. Echolalia disappears if the child begins to understand the speech of others. In some cases of IA, there are pronounced articulation disorders; labial sounds (M, P, B) are more often affected.
Some children repeat questions addressed to them very quickly and only after saying the question do they understand the interlocutor. In this case, an adaptive system of understanding probably develops, in which repetition and pronunciation play an intermediate role.
N.N. Traugott [6] described a situation where a person suffering from alalia understood and followed verbal instructions if the reward for the answer was candy, which the boy liked, but ceased to understand if the type of candy was changed. As a result of the research, she came to the conclusion that the child understood the addressed speech when he wanted. A.L. Bitova and E.N. Safronova [36] note that a child with sensory alalia does not use hearing at all or uses it under conditions of overmotivation, when the child really needs to understand something. Their parents also describe the behavior of children with IA: the child either understands speech or behaves like a deaf person. In our opinion, in children with IA, involuntary understanding of the speech of others is impaired or later formed, which ensures the development of their native language. Voluntary understanding becomes possible after 3 years. Later, when the child already has some vocabulary, the dependence of understanding on voluntary attention is clearly visible.
There are different variants of the course of IA.
Spontaneous compensation of the defect. In this case, at some stage of development, the child begins to understand the speech of others, an impressive vocabulary develops, and then the formation of spoken language occurs. In this way, IA syndrome is similar to SLS. In all cases of IA known to us, when involuntary understanding of speech at some point became possible, and one’s own speech began to develop (4 patients out of 17, i.e. 23.5%) and the clinical picture of speech underdevelopment acquired features of one form or another EA.
Observation 3
Boy, 3 years old, from a Russian-speaking family living in Germany. The anamnesis is not burdensome. Parents note lack of speech; hearing is normal.
Severe IA: the child did not comply with verbal requests, did not speak, did not repeat, and accompanied the game with quiet babbling. He understood and followed gesture instructions. Behavior is adequate, calm, assiduous.
Examination six months later: he easily understood many questions: “what is your name,” “what is the name of your mother and brother,” and answered them. Showed body parts and surrounding objects by name. He immediately turned around when his name was called. I listened to a story based on a series of pictures. Passive vocabulary is poor. He answered questions and expressed desires, usually in one word. If words were not enough, he used gestures. Expressive alalia was diagnosed. Subsequently, the boy studied with a Russian speech therapist. He began to speak in phrases; the most persistent symptoms of speech underdevelopment were agrammatism (speaking without endings) and insufficiency of auditory-verbal memory. The boy attended a German kindergarten and mastered the German language. They spoke Russian at home, meaning the boy became a natural bilingual. At the age of less than 7 I went to a German general school, and in the first grade my academic performance was normal.
Observation 4
Girl, 3 years 11 months, from a Russian-speaking family living in Germany. Hearing is normal. At the time of examination, she spoke individual words, rarely phrases of 2-3 words, the vocabulary was poor and covered only the most necessary everyday concepts. She spoke without endings, her pronunciation was unclear. At the same time, the girl demonstrated good cognitive activity: she carefully looked at books with pictures and easily put together puzzles; At the same time, I didn’t want to listen to the story from the pictures, I tried to understand the plot with my eyes. She often did not respond to verbal requests; echolalia.
Positive dynamics were noted during the classes. After 1 year, the girl demonstrated satisfactory understanding of speech in the process of completing tasks, but it was almost impossible to attract or switch the child’s attention with verbal instructions, auditory attention remained reduced: the question had to be repeated several times. Agrammatisms persisted. The pronunciation became intelligible, only individual sounds (L, R, CH) were distorted. Later, the girl began to attend a German kindergarten, and at the age of 6 she went to a German general school. Natural bilingual. She studied with a German speech therapist and noted pronounced agrammatisms.
The above clinical observations suggest that with IA there may be a delayed development of the function of involuntary speech understanding. The “turning on” of the function of understanding occurs, apparently, gradually, and for a long time it can remain a weak link, subject to exhaustion. After speech understanding becomes available, the picture of its underdevelopment takes on the features of E.A. The most persistent symptoms are impressive agrammatisms, inability to distinguish close-sounding phonemes and insufficiency of auditory-verbal memory. Involuntary understanding of speech remains inaccessible; the child is forced to rely only on voluntary understanding.
After 3 years, there comes a time when the child begins to point to objects or pictures, as if asking - what is this? And listens to the names. At this moment, voluntary attention is activated and the meaning-sound connection can be established.
Observation 5
Boy, 4 years old, from a Russian-speaking family living in Germany. Parents' complaints about their child's lack of speech. Hearing is normal. History of complications during childbirth. The mother demonstrated the child’s understanding of several words: the boy showed pictures in the book by name. However, he did not respond to questions or calls by name, could not point out objects in the office by name, or choose one of the three proposed toys. The child was calm, assiduous, and performed tasks that did not require verbal understanding. He communicated with gestures and quiet exclamations. He repeated the vowel sounds A, I. He could not repeat syllables and words. Diagnosis: impressive alalia.
Subsequently, the child studied with speech therapists, attended a German kindergarten, then a German general school, but did not master the German language. The boy's parents transferred him to a school for children with developmental disabilities. I understood only a few German words that I learned at home. When examined at the age of 10, he quickly and quietly repeated questions asked of him and then answered. He answered only the simplest questions without repetition. In many cases, after repeating the question, I could not answer (for example, the question: what floor do you live on?). While listening to the questions, I looked carefully at the interlocutor’s face. The boy had a fairly extensive vocabulary and could name pictures that depicted one action. It was not possible to compose a story from a picture depicting several characters. Could list items belonging to a certain category. The pronunciation is clear, but there are substitutions of sounds, most often deafening of voiced consonants. I tried to use gestures to communicate; only at the persistent request of adults did I use memorized phrases.
Observation 6
Boy, 9 years 5 months, from a Russian-speaking family. He spent the first years of his life in Russia. The child did not speak on time, but speech therapy classes were not conducted. According to the mother, behavioral disorders gradually became so pronounced that she was afraid to leave the house with her son. When the child was 8 years old, the family moved to Germany, and the boy began to attend a school for children with reduced intelligence, but by this time his behavior had returned to normal. At school I began to learn German. During the examination: the boy did not pay attention to verbal addresses, did not react to vocative intonation, but non-verbal contact was good, the child readily completed tasks. When concentrating, he could show some objects by name; the passive vocabulary is extremely poor. To communicate with the family, I used several Russian phrases - when pronouncing them I was unsure, agrammatisms were noted, many sounds were distorted.
In the last two cases, there was no spontaneous development of the function of involuntary speech understanding. Probably, in the case when involuntary understanding of the speech of others becomes possible even in the preschool period, one can expect delayed but full-fledged language acquisition. A later “switching on” of understanding may not lead to a noticeable improvement in language function, since over time, thanks to plasticity, an adaptive functional system of speech understanding develops (for example, through repetition of a question). In addition, the ability to acquire a language declines with age. The child must be immersed in a language environment (meaning the first language) no later than 5-7 years, otherwise there may not be full language development [37, 38].
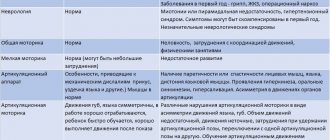
The table compares the main characteristics of language acquisition by healthy children and children with AI.
Comparison of language acquisition in healthy children and children with IA
Mastering a native language is a natural state of a developing individual, i.e., this process develops as an independent behavior [9, 39]. Speech understanding during language development in healthy children always precedes speaking skills [35]. Undoubtedly, this understanding is involuntary. The most important feature of mastering one’s native language is the path from understanding entire statements to understanding individual units of language. So, L.S. Vygotsky [40] wrote that the child begins with the whole in the development of the semantic side of speech and only later moves on to mastering particular semantic units, individual verbal meanings. The first words that a child utters can be considered in meaning as equivalent to phrases [41]. The literature [19] emphasized that language is not a disparate set of units, but a complex of interacting processes that allow it to act as an integral system.
There are two ways of mastering a language - natural (this is how the first native and subsequent languages are mastered when immersed in a living language environment) and learning in a logical way (the result is a foreign language). Both methods interact in healthy people and allow the acquisition of new languages in different conditions and at different ages, but can also function independently. The features of learning a foreign language coincide with the features of language acquisition by children with a severe form of I.A. A child with IA cannot master the language on his own and without proper pedagogical support he remains without it. For comparison: with EA without pedagogical assistance, language acquisition is possible, only individual elements suffer.
Studies of the role of genetic factors in the etiology of underdevelopment of oral speech [1] show that they play the greatest weight in cases of selective, uncomplicated forms of underdevelopment of expressive speech (EA), which usually lead to impairments of moderate severity with a relatively favorable prognosis for compensation.
The idea of IA as a disorder in which it is impossible to master a language as a native language, but it is possible to study it as a foreign language, is, according to our observations, very productive. This idea provides a certain basis for planning pedagogical assistance to children with this syndrome, on which specific methodological techniques can be built that are appropriate to the age and characteristics of the child. This idea also helps parents understand the logic of this syndrome and the difficulties experienced by the child, which is necessary for organizing classes at home.
When organizing pedagogical assistance, the issue of using the auditory modality is controversial. In the auditory modality, work should be based on voluntary auditory attention, which is preserved in this syndrome. In this case, it is necessary to take into account the exhaustibility of voluntary attention and use other, intact analyzers.
Diagnosis of IA is difficult for a number of reasons. Firstly, it is possible to verify whether a child understands speech or not only by the child’s external manifestations and behavior. However, a healthy child of 2-3 years old may not turn around when called by name because he does not want to communicate with this person, is shy, or is completely absorbed in the game. Impaired communication ability is observed in autism spectrum disorders. With severe behavioral disorders, which can be either isolated or accompanied by IA, it is very difficult to establish non-verbal contact with the child; this sometimes requires several meetings. Therefore, in our opinion, the most important condition for diagnosing IA is reliable contact with the child on a non-verbal level. It is the difference in the execution of verbal and non-verbal commands that serves as a diagnostic criterion.
Differential diagnosis of IA and hearing impairment is described in detail in the works of N.N. Traugott [6, 20], as well as L.G. Paramonova [2]. Assessing speech understanding in children in multilingual environments is especially difficult. As a rule, children 2-3 years old who are in contact with several languages know some words and commands in one language, and some in another. In a multilingual environment, one can often observe the phenomenon of non-pathological erasure of language ( English:
language attrition): a child easily forgets one of the languages if the intensity of communication in it decreases. However, a healthy child never loses the ability to verbally communicate: he either changes one language to another, or becomes monolingual from bilingual. When diagnosing language impairment in a multilingual environment, it is advisable to test all languages with which the child is exposed. Many observations of the development of speech in healthy children in a bilingual environment record one or another delay in language development during the transition to phrasal speech. It is very difficult to understand what is causing the lack of language development in these cases.
Differential diagnosis of IA and early childhood autism is often difficult. According to H. Amorosa, M. Noterdaeme [42], such a diagnosis is impossible at an early age, but later, as the child develops, it is not difficult. Often the same non-speaking child of 2-3 years old makes a different impression on different days. Moreover, even during one lesson, the child’s condition may change.
With IA syndrome, involuntary speech understanding, which is normally the basis for mastering the native language, is impossible due to a pathology of unknown origin. At the 4th year of life, voluntary understanding becomes possible. For healthy children, voluntariness is an additional tool in understanding the world and language, and for children with IA it is the only possible way to understand the speech of others.
Summarizing the analysis of the literature, clinical observations, as well as the results of comparison of symptoms, course, outcomes and dependence of language syndromes on the age of children [43], we can draw the following conclusion: many cases of IA are based on functional brain damage. In essence, dysfunction is a pathological process that does not destroy the brain, but complicates or makes impossible the functioning of its individual regions and the normal development of cognitive functions. Clinical manifestations depend on the area of the brain affected by dysfunction and, apparently, can be similar when exposed to various pathogenic factors. In the development of speech pathology in dysfunctional disorders, the intensity of the pathological process can play a greater role than its localization. S.B. Buklina et al. [44] noted that in epilepsy, not only focal “disconnections” of functionally significant areas are possible (for example, leading to the appearance of aphasia), but also a global restructuring of functional systems. Dysfunctional disorders can lead to permanent impairment of speech and other cognitive functions. At the same time, spontaneous restoration of impaired functions is possible. The prognosis depends on the duration of the pathological process. Plasticity in dysfunctional disorders manifests itself either as the elimination of dysfunction (the functioning of the affected regions spontaneously normalizes, cognitive functions are restored) or the formation of workarounds for verbal communication (for example, understanding speech through repetition in IA).
We make assumptions about the possible dysfunctional nature of IA based on: 1) the persistence of IA symptoms; 2) the identity of the symptoms, course, and outcomes of IA and SLK, the dysfunctional nature of which is known; 3) differences in symptoms, course, outcomes and age dependence from childhood aphasias due to damage to the brain substrate and SLC [43].
In some cases of IA, it can be assumed that there is a disruption in the maturation of brain structures responsible for the formation of language. The cause may be pathology of the pre-, peri- and postnatal period. In these cases, the nature of the course of the syndrome - a consistent improvement in auditory perception - is closer to the course of syndromes due to pathology of the brain substrate. Suggestions have been made [4] about the connection between the pathology of the corpus callosum and I.A. syndrome. Perhaps the plasticity of the brain, which is so clearly manifested in cortical brain lesions, does not extend to subcortical structures.
“Language Bridge” is a public, non-profit organization whose goal is to promote German-Russian bilingualism, as well as language therapy.