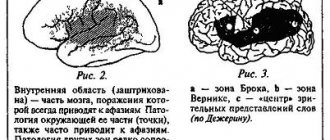
Motor cortical aphasia (Broca), verbal, expressive aphasia
Motor cortical aphasia is characterized by impairment of oral speech, writing, and reading. Motor cortical aphasia occurs when the posterior parts of the inferior frontal gyrus of the dominant hemisphere are damaged. In mild forms, speech is slow, ungrammatical, the construction of phrases is impaired, and the set of words is reduced. Synonyms for motor cortical aphasia are Broca's aphasia, verbal aphasia, and expressive aphasia. With severe disorders, patients use only a few words or syllables (speech embolus) to express various shades of their emotions.
Sensory cortical aphasia, Wernicke's aphasia, word deafness
Sensory cortical aphasia has several synonyms - Wernicke's aphasia , word deafness . Sensory cortical aphasia is characterized by a lack of understanding of the normal correct speech of others with preserved hearing. Patients with sensory cortical aphasia speak a lot, but their speech consists of a random collection of words and sounds. Sensory cortical aphasia is observed with damage to the posterior parts of the superior temporal gyrus of the dominant hemisphere. Sensory cortical aphasia is often combined with acalculia.
How to treat aphasia, get rid of aphasia?
Sarklinik knows how to treat aphasia , speech disorders characterized by partial or complete loss of the ability to use words and phrases, how to get rid of aphasia in Saratov. A variety of reflexology treatment methods have helped many of our patients get rid of aphasia in right-handed and left-handed people. Effective treatment of aphasia gives excellent results; patients (children and adults) restore lost speech abilities and begin to understand their thoughts and the speech of others. On our website sarclinic.ru you can see a doctor for free and get a short answer on the treatment of aphasia.
Definition of aphasia
Literally, the term aphasia is translated from Greek as “I don’t speak.” As a rule, this pathology occurs in the adult population, but it is quite possible for it to develop in children whose speech has more or less developed, that is, from three years of age and older.
In clinical neurological practice, the term aphasia has the following meaning: it is a disorder of speech function of a systemic nature, consisting of either partial or total loss of formed speech function. This definition implies the presence of a defect in the central nervous system, the presence of damage to the speech zones of the cerebral cortex and the resulting speech disorders that affect both internal and external speech.
Clinically, aphasia can have varying degrees of severity and, as a rule, is not the only or isolated manifestation of brain damage. Moreover, its development and severity depend on the location and volume of the lesion.
Treatment of aphasia in Saratov, Russia
At your first consultation you will receive information about the treatment of aphasia and the following questions. Semantic and traumatic aphasia. How does speech restoration occur in aphasia? How does speech sound in patients with aphasia? What is optic-mnestic aphasia, afferent and efferent aphasia, dynamic acoustic-gnostic and acoustic-mnestic kinesthetic aphasia? How are stroke (a condition after a stroke), alalia, agnosia, apraxia and aphasia disease related and how do they differ? How are patients examined and speech therapy work done for aphasia? Why do you need an aphasia speech map? What exercises should you do for aphasia?
Sign up for a consultation. There are contraindications. Specialist consultation is required.
Photo: Santos06 | Dreamstime.com\Dreamstock.ru. The people depicted in the photo are models, do not suffer from the diseases described and/or all similarities are excluded.
Related posts:
Intracranial hypertension syndrome, liquorodynamic disorders
Agrammatism, paragrammatism, dysgrammatism
Akataphasia, treatment of akataphasia in Saratov
Psychopathy, types, symptoms, treatment of psychopathy in children and adolescents
Neuroses in children, childhood neurosis, treatment of neuroses
Comments ()
Speech examination “Diagnostics of aphasia”
EXAMINATION OF DISTURBED
HIGHER CORTICAL FUNCTIONS
Like any speech therapy examination, examination of speech in aphasia begins with a preliminary conversation that allows establishing contact with the patient, assessing:
1) speech capabilities,
2) preservation of consciousness,
3) criticality,
4) orientation in the environment, in location, in time.
The patient is asked questions about his well-being, the time of year, the date of his illness, his educational level, specialty, marital status, the presence of left-handers in the family, etc. are found out.
Determining the presence of left-handedness
:
1) interlacing of fingers.
2) crossing arms over the chest (for a left-handed person, the left hand lies on top);
3) aiming when simulating archery.
4) along the venous network (brighter on the leading arm)
Examination of non-speech praxis and gnosis
is carried out using non-speech examination methods, which make it possible to identify the integrity or impairment of the parietal lobe, posterior frontal and premotor parts of the occipital regions.
Dynamic Praxis Research
is carried out by patients performing imitation, and then following an oral task, tests
for switching from one movement to another.
The patient holds his hands on the table and simultaneously changes their position.
In the presence of dynamic premotor apraxia,
the patient begins to repeat the same movement with one hand or another, loses rhythm (
reciprocal test)
. The “fist-rib-palm” test is designed to study the integrity of the movement plan
.
In the presence of premotor apraxia,
the patient does not maintain the plan of movements, skips and repeats individual movements.
The presence of dynamic apraxia
indicates the presence of a lesion in the premotor and posterior frontal regions, and in some cases in the subcortical regions of the cerebral cortex.
Spatial Praxis Survey
allows us to judge the safety or disruption of complex simultaneous syntheses. In patients with extensive damage to the upper nonparietal parts of the brain
There may be signs of spatial disorientation in everyday life. Patients cannot find their room, cannot dress properly, etc. The following tests are offered:
- Head's samples. The patient is asked to imitate the following movements together with the speech therapist: bring the index finger to the chin, turn the hand palm up and fingers away from the chin, place the left palm perpendicular to the chin, place the palm perpendicular to the other palm, etc. The patient’s orientation in the left and right side of the body.
- Copying by the patient various figures made from matches, folding them upside down, the KOOS technique. In addition, the patient’s reproduction of symbolic movements is examined: the patient is asked to wag his finger, beckon someone to come to him, clap his hands, depict cutting paper, cutting bread, etc.
- Test with a clock and a geographical map. The patient is asked to determine the time on a drawn clock without numbers in the direction of the arrows; draw arrows conveying this or that time; find seas, cities, countries on the map; mark the location of north and south, east and west on the axes crossed perpendicularly; draw the contours of the Black Sea, etc.
4. The patient’s orientation is checked among letters written correctly, mirror and horizontally on the line.
Difficulties in performing these tests are typical for patients with afferent and semantic aphasia
, i.e., with damage to the posterior inferior parietal parts of the brain.
When the premotor and posterior frontal
parts of the cerebral cortex are damaged, inertia and impaired planning of actions and movements are revealed when performing a series of these tasks.
Rhythm evaluation and playback
The patient's ability to motor switch from one rhythmic pattern to another and the tendency to simplify the rhythmic pattern are checked. The speech therapist taps the rhythm on the table with a pencil, covering it with a sheet of paper, two or three beats at a time, in different series: two strong, two weak, two fast, one delayed, etc.
Patients who do not maintain a given rhythm, automatically add, repeat one group or series of beats, or add extra beats, repeating them due to perseveration, belong to the group with damage to the premotor and posterior frontal parts of the cerebral cortex. Patients with sensory aphasia
refuse to play rhythmic beats, stating: “There are a lot of them.”
Patients
correctly reproduce rhythmic patterns from auditory imitation, but cannot describe the nature of the rhythms.
Visual gnosis examination
carried out to distinguish speech disorders from naming difficulties with visual agnosia that occurs with damage to the tertiary parts of the occipital lobe and to clarify optical alexia that occurs with damage to the parietal parts on the left. The patient is asked to name or describe objects or their images. He is given simple, clear, contrasting object pictures, then similar in shape (ball, apple, globe, glasses, bicycle, etc.). Then they are replaced by single-color, contour, speckled (covered with small dots), crossed out with zigzag lines and contour images superimposed on each other. Patients with visual agnosia have difficulty recognizing and describing the functions of objects.
Letter recognition
written in different fonts is tested in well-speaking patients by naming them and showing them according to instructions. Patients with optical alexia have difficulty completing these tasks.
Oral and facial praxis examination
Violation of oral and facial praxis
often combined with a violation
of articulatory praxis
. Oral praxis includes non-speech movements of the oral apparatus, i.e. lips, tongue, cheeks.
The study consists of the following tests:
- the patient is verbally given instructions to open his mouth, stick out his tongue, lift it up, down, move it to the left, to the right, click his tongue, put his tongue behind his cheek, inflate his cheeks alternately and at the same time, stretch his lips forward, stretch his lips.
- The patient performs the same tasks by sightsolid imitation
.
- Next, according to the oral task and visual imitation, various symbolic movements
: blowing, imitation of spitting, whistling, imitation of gargling, coughing, reproducing a smile, raising eyebrows as a sign of surprise, winking, etc.
The patient performs all these tests in isolation, with pauses between tasks. Difficulties in performing these tasks in different localizations manifest themselves in different ways. For pseudobulbar dysarthria
profuse salivation, viscosity, incomplete movements, and changes in facial expressions appear.
With lower parietal lesions,
various chaotic searches arise and difficulties in giving the articulatory organs the appropriate positions.
Patients with oral, inferior parietal apraxia
cannot voluntarily depict the movement of a kiss or spit according to instructions, while these movements are preserved in everyday life.
Oral, inferior parietal apraxia
in some cases is observed in isolation, without speech disorders.
When the premotor and posterior frontal areas are damaged
, perseverations, repetitions of previous movements, and difficulties in performing serial tasks occur.
To test dynamic oral praxis, the patient is asked to perform a series of movements, such as blowing and flicking the tongue. Patients with premotor apraxia
perform individual movements well and get stuck on one of the movements included in a linearly organized series of movements due to perseveration.
At the same time, sometimes there is an illusion of the presence of simultaneous , constructive, spatial apraxia
with damage to the premotor parts of the cerebral cortex.
In case of extensive lesions of the frontal lobes,
due to severe inactivity and spontaneity, involuntary spitting and coughing are impaired, while the performance of these movements is relatively intact when stimulated.
Examination of speech functions
Examination of speech functions
covers
all types of impressive and expressive human speech activity,
this includes:
1) indicative examination of spontaneous speech
(during
a preliminary conversation with the patient)
. The speech therapist records the activity and volume of the patient’s speech production (when examining a speechless patient, the speech therapist notes whether he is active, whether he is trying to answer questions with the help of emboli, whether his speech is sufficiently colored with various intonation shades or whether he is indifferent).
2) examination of speech understanding.
Before proceeding with the examination of understanding, the speech therapist needs to make sure
that the patient’s hearing is intact
, and also find out how many times he has had cerebrovascular accidents and what they were accompanied by.
3) examination of phonemic hearing.
The patient is asked
to repeat close (oppositional) phonemes
: for example, on
b
, raise your hand, and on
p
, keep your hand on the table, then a series of syllables ba, pa, pa, ba, pa is given. Finally, phonemic awareness can be explored by showing appropriate syllables or words with opposition sounds (house-tom, barrel-kidney).
For severe acoustic-gnostic sensory aphasia
at an early stage after a stroke, patients do not distinguish even phonemes that are distant in sound, later - only phonemes that differ in one acoustic feature: voiced - unvoiced, hard - soft, whistling - hissing.
Phonemic hearing is secondarily impaired in gross afferent motor aphasia
due to a violation of kinesthetic afferentation.
Patients do not distinguish by hearing phonemes that are close in place and method of articulation (m - b - p, n - d - t - l) both in the perception of syllables and in the perception of words, however, phonemic hearing is
less impaired
in afferent motor than in acoustic-gnostic aphasia
.
With pronounced efferent motor aphasia
, perseverations occur during the study of phonemic hearing.
4) examination of
understanding meanings .
During the examination, the patient is asked to show objects surrounding him (table, chair, book, pencil, window, door, ceiling, steps, closet, etc.), to show parts of the face and body.
Difficulties in showing parts of the body and objects in the room are observed in all forms of aphasia: in sensory aphasia - due to impaired phonemic hearing and instability of auditory-verbal traces; with efferent - due to the presence of perseveration in hand movements; with afferent and semantic - with rapid presentation of words due to difficulties in orientation in space.
Hearing-verbal memory impairments
are identified by the patient repeating a series of words (two, three or more), for example, house - cat - forest, hand - window - fish, etc. Patients are given the task to repeat the sentence.
Apple and pear trees grew in the garden behind a high fence. Patients with acoustic-mnestic aphasia,
unable to retain the speech sequence, usually miss the second and third words;
with efferent
patients persist the first or second word, as well as words from previous tasks.
Another technique for examining auditory-verbal memory
is to find,
laid out in front of the patient or
Secondarily, mild auditory-verbal memory can be impaired when both the frontal lobes of the brain and the inferior parietal parts of the left hemisphere are damaged in right-handed people.
5) examination of understanding of simple sentences:
1) the patient’s understanding of simple and relatively complex instructions such as Take a pencil, put it under the book, and give me the scissors;
2) understanding of sentences, names, names of objects given in the form of descriptions.” Show what they use to cut bread, what they use to cut paper, what they use to light firewood, etc. (according to the corresponding pictures).
Difficulties in understanding multi-unit instructions are observed in all forms of aphasia with severe speech disorder.
6) examination of the understanding of grammatical structures,
proverbs, sayings, fables.
The patient is presented with the following tasks: Tell me, how do you understand the phrases “father’s brother” and “brother’s father”? Is this the same person or different people? If different, then who are they?
When showing the corresponding pictures, the speech therapist asks the patient to show
his mother’s daughter, daughter’s mother, daughter’s mother, mother’s daughter
.
In the same way, but relying on objects, the patient is asked to show a brush with a pencil, a pencil with a brush.
Testing the understanding of logical and grammatical constructions that convey the spatial arrangement of objects
, carried out by tasks: Place the pen to the right of the ruler and to the left of the pencil, the ruler to the left of the glasses correction key, etc.; Draw a cross under the circle, a circle above the cross, a cup under the table and above the Christmas tree, etc. To make the task easier, the patient is given schematic examples of these drawn objects.
When solving a task of a defining nature, the patient is asked to place the names of the children under the pictures: Kolya is higher than Vanya and lower than Sasha. Who are Kolya, Vanya and Sasha here? Or: Olya is darker than Katya and lighter than Tanya. Which of the girls is Olya, Katya and Tanya? Petya hit Kolya. Who's the fighter?
These tasks are difficult with afferent aphasia, and the instructions: “Show the spoon with a pencil, the pencil with a pen,” etc. are difficult with efferent aphasia.
Patients with semantic aphasia are characterized by difficulties in performing both logical and grammatical constructions.
7) examination of expressive speech
begins already during the preliminary conversation. The speech therapist writes down all his questions and tasks, as well as the patient’s speech and facial reactions, for example, in the form of a fraction: above the line is a question, the content of the drawing about which the patient must report something, below the line is the patient’s speech production.
Examination of the articulatory part of speech
The articulatory link can be disrupted in different types of afferent motor and efferent motor aphasia, with dysarthria
.
The patient is asked to repeat the sounds in isolation, in words, in a sentence. With gross afferent motor aphasia,
either abundant searches for the articulatory structure of sound, or literal paraphasias, or replacement of the pronunciation of individual sounds with speech emboli can be observed.
The patient either pronounces sounds correctly, then replaces them with others, or cannot find the desired articulatory position. With relatively restored situational speech (for example, with so-called conduction aphasia), patients may have difficulty pronouncing individual sounds, but more often - when pronouncing syllables and words. With grossly impaired phonemic hearing in patients with acoustic-gnostic aphasia,
errors may also be observed when repeating individual sounds.
Moreover, these difficulties are accompanied by comments from patients. Difficulties in repeating individual sounds
in
sensory
are secondary in nature and are a consequence of impaired auditory control.
One of the features of the repetition of individual sounds in
afferent motor and acoustic-gnostic sensory aphasia
is the tendency to deafen voiced phonemes,
in afferent motor aphasia there is a tendency
to voiceless phonemes,
in acoustic-gnostic sensory aphasia
there is a tendency to deafen the phoneme,
in afferent motor aphasia
there is due to apraxia of the vocal cords, a tendency to voicing in acoustic-gnostic aphasia is due to an increased compensatory pre-superstructure of acoustic control.
Examination of automated types of speech
The patient is invited, together with the speech therapist, to sing the melody of a familiar song (with and without words), repeat the singing independently, list the days of the week, months of the year, and reproduce the ordinal count. If this is not available to the patient, then the words are pronounced in conjunction with it.
Examination of conjugate and reflected repetition
allows us to clarify the degree of decay of phonemic hearing, auditory-verbal memory, articulatory praxis and the presence of perseveration in the speech of patients.
Patients are given the task to repeat several one-syllable, two-syllable, three-syllable and polysyllabic words of varying frequencies, as well as repeat phrases of varying lengths.
Examination of the nominative function of speech
Naming refers to reproductive, voluntary types of speech (repetition, dictation, reading aloud). Therefore, when starting the examination, the speech therapist asks the patient to name objects or images in one word, to find a categorical name (dishes, furniture).
Examination of dialogic and monologue speech
(preliminary conversation) The speech therapist notes whether the patient is verbose or not. How developed is his speech, does he speak in monosyllables, in separate lines, or uses cliche-like turns of phrase? Is there agrammatism in his situational speech, what is the nature of this agrammatism. To examine narrative speech, the patient is asked to compose sentences or a story based on plot pictures.
When recording the patient’s speech, the speech therapist notes the nature of the patient’s agrammatism, the richness of his vocabulary, verbal and literal paraphasias, preservation of the narrative plan, etc. With severe afferent and efferent aphasia, the patient’s narrative speech may be completely absent, and at an early stage with acoustic-gnostic aphasia be overloaded with literal paraphasias.
Examination
of the state of reading and writing
When examining the state of reading, special attention is paid to the possibility of internal reading
in speechless patients with afferent and efferent motor aphasia and sensory and acoustic-gnostic aphasia. Examination of the safety of internal reading to oneself in speechless patients is carried out using the following methods: 1) laying out captions for objects, plot pictures and series of pictures; 2) showing a word or sentence perceived by ear; 3) following written instructions: Show where the window is, Wag your finger, etc.
In patients complaining of reading difficulties with intact situational speech, it is necessary to check visual acuity and optical gnosis, the presence of hemianopsia (narrowing of the visual field, often observed in sensory aphasia). When studying reading capabilities in patients with moderate severity of speech disorders, the speech therapist notes literal and verbal paralexias, elements of guessing reading, perseveration, etc.
When examining writing and written speech, patients with severe speech disorder are asked to write individual sounds and short words under dictation (house, ear, window). In cases where the patient can cope with writing easy words, he is asked to write down words with consonant clusters (tail, friend, table) and polysyllabic words (for example: room, plane, chase). If the patient writes (with errors) individual words, he is asked to take dictation of simple and complex sentences, for example: Children go to the forest. The weather is bad outside, the journey ended well.
For mild speech disorder
There are errors in patients' letters. If the patient did not make mistakes when writing from dictation, it is necessary to move on to the study of written naming, composing a phrase or text based on plot pictures.
Impairments in written speech in all forms of aphasia are secondary to the primary disorder. In the written speech of patients with afferent motor aphasia, literal paraphasia is predominantly observed when recording sounds that are close in place and method of formation; in efferent aphasia - omission of vowels, rearrangements and perseveration of letters and syllables from previous words; in acoustic-gnostic aphasia - mixing of voiced and voiceless consonants etc. With rough and moderate severity of agraphia with afferent motor, efferent motor and acoustic-gnostic aphasia, omissions of consonants are observed at confluences of consonants in a syllable or at the junctions of syllables. In severe acoustic-gnostic aphasia at the very early stage of the disease, due to impaired auditory control, the patient can write extra letters in a word, repeat syllables, lengthening, for example, a word consisting of three letters to 8-12 letters. The speech therapist records the patient’s written speech also in the form of a fraction.
And finally, the speech therapist examines the patient’s integrity of counting operations
, offering to write down simple and multi-digit numbers, solve examples within 10, 100, 1000. Usually, seriously ill patients are given written examples like: 31 -17 (with a transition through ten), patients are asked to verbally subtract from 100 by seven, etc.
The examination of speech functions is carried out delicately
In order not to injure the patient, the patient is encouraged to overcome difficulties during the examination. The patient should leave the speech therapist encouraged, not overtired, and therefore the initial examination is carried out in a reduced manner and the speech status is clarified during repeated meetings.
Conclusion about the patient’s speech status
1) emotional and volitional traits of the patient, contact, integrity of personality, his orientation in place and time, attitude towards his speech defect, the presence of left-handedness in the patient and family members;
2) features of understanding situational speech, implementation of single- and polysyllabic instructions, auditory-speech memory, phonemic hearing, alienation of the meaning of a word, perseveration in completing tasks, understanding of logical-grammatical structures;
3) features of expressive speech: verbosity, aspontaneity, echolalia, perseveration, speech emboli, the nature of agrammatism, the presence of verbal and literal paraphasia, amnestic difficulties, oral or articulatory praxis. Possibilities of repetition, naming, composing phrases, automated speech. Is there a dissociation between reproductive voluntary and situational active speech, as well as the presence of dysarthria?
4) features of reading and writing: preservation of visual gnosis, letter recognition, features of reading silently and aloud, literal and verbal paraphasias, the ability to follow written instructions, global reading of individual words;
5) features of written speech disorders: writing individual letters, words under dictation, writing naming objects and their images, writing complex words and individual sentences under dictation, writing sentences based on a plot picture, the nature of literal and verbal paraphasia, agrammatism in written speech, character other defects in the patient's letter;
6) features of counting disorders: the ability to solve various arithmetic examples, write numbers under dictation;
7) features of gnosis and praxis: the presence of acoustic or optical agnosia, specularity in writing, oral and articulatory apraxia, dynamic and constructive-spatial apraxia, dysarthria, echolalia.
After a summary description of the patient’s speech status, a conclusion
, which notes
the form of aphasia, its degree of severity, the complexity of the two forms, the severity of agraphia, alexia, the nature of apraxia, the presence of left-handedness in the family, the degree of activity or aspontaneity , the presence of depression, efficiency, weak soul , disinhibited femininity).